Introduction
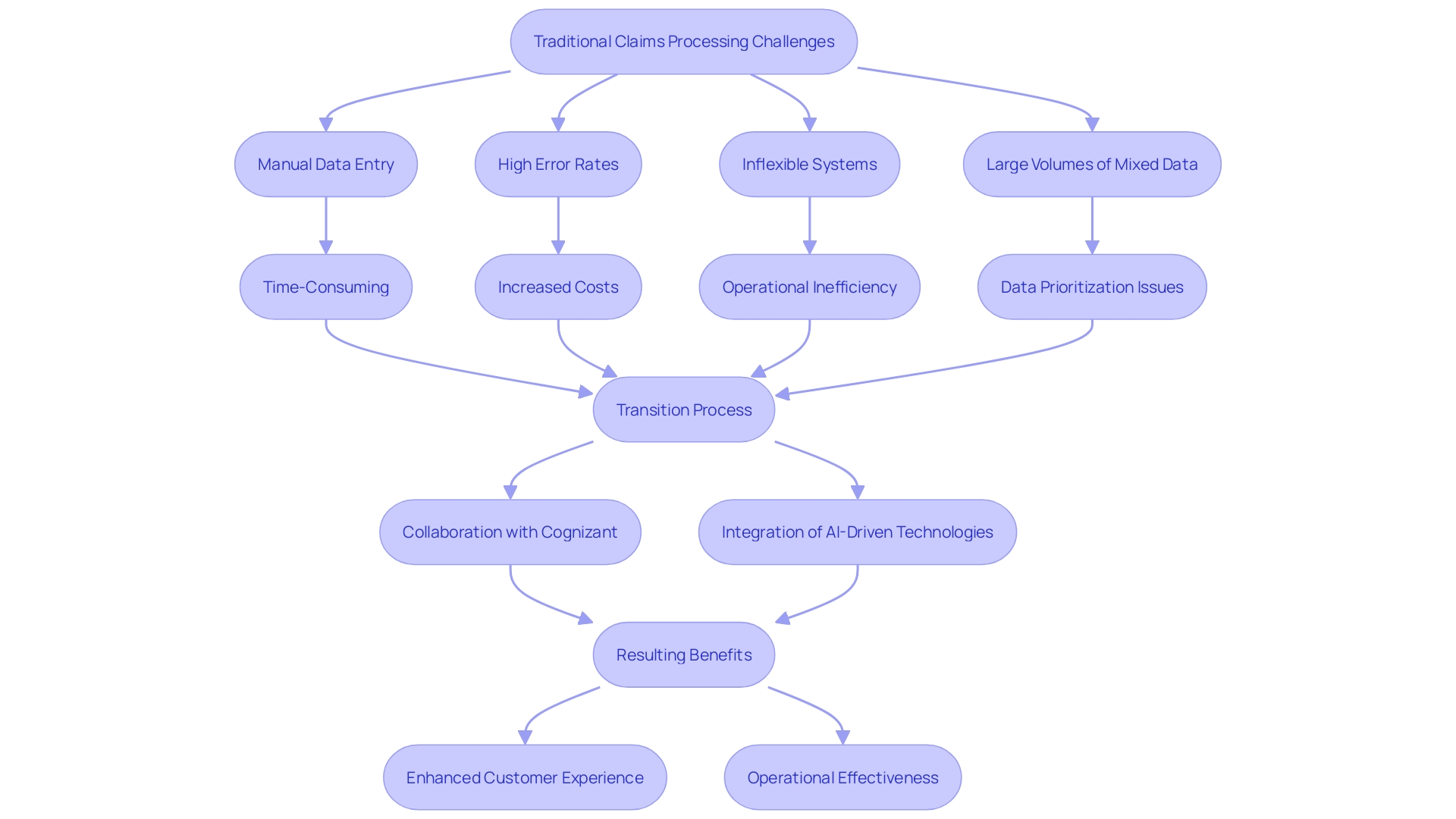
In the ever-evolving landscape of insurance, traditional claims processing methods face mounting challenges that hinder efficiency and customer satisfaction. Manual data entry, extensive paperwork, and prolonged response times result in high error rates and increased operational costs. To navigate these complexities, forward-thinking companies are embracing automation technologies to transform their claims processing systems.
This article explores the pivotal role of AI and automation in revolutionizing the insurance sector, highlighting real-world case studies and the substantial benefits of automated claims processing. By examining the key technologies driving this transformation, such as Optical Character Recognition (OCR), Natural Language Processing (NLP), and Robotic Process Automation (RPA), the discussion will underscore how insurers can achieve remarkable improvements in efficiency, accuracy, and customer experience. Moreover, the insights and best practices shared will guide organizations on their journey to digital transformation, ensuring they remain competitive in an increasingly demanding market.
Challenges in Traditional Claims Processing
Traditional claims processing is plagued by manual data entry, extensive paperwork, and prolonged response times, leading to inefficiencies and increased operational costs. This outdated approach lacks clarity, resulting in high error rates and reduced client satisfaction. The dependence on legacy systems further complicates the adaptation to changing client expectations and regulatory requirements. Forward-thinking companies are now turning to automation to address these challenges. For example, Cognizant’s collaboration with Alm. Brand Group in Denmark is a testament to the transformative potential of automation. By automating various insurance policies and administrative tasks, they aim to enhance efficiency, improve customer experience, and boost competitiveness. As emphasized by industry specialists, AI-driven technologies such as generative AI can greatly update the process by searching, generating, and summarizing information swiftly and precisely. This shift not only streamlines workflows but also enhances productivity and operational efficiency, fundamentally changing how insurers manage and process requests.
The Role of AI and Automation in Claims Transformation
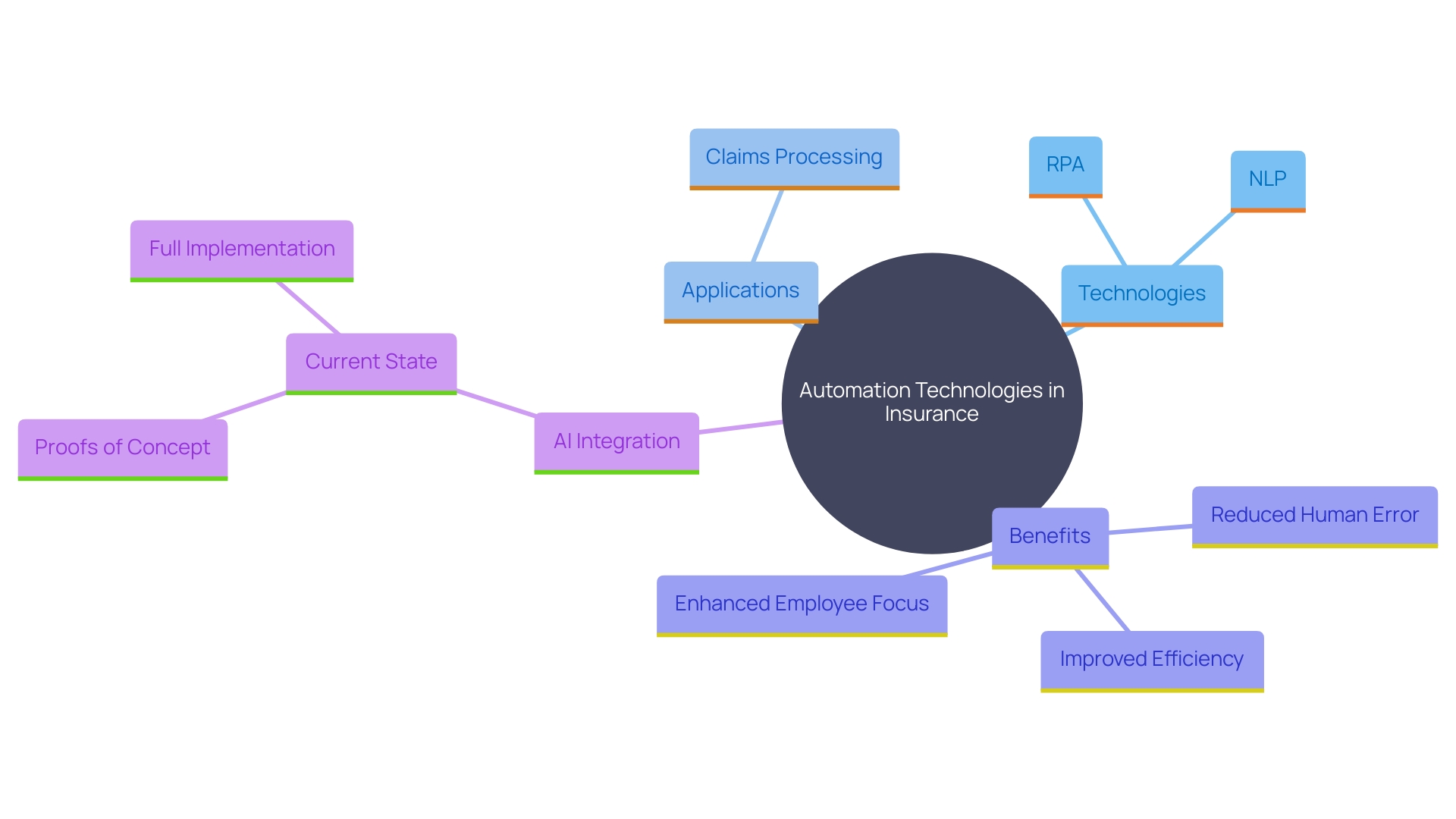
Automation technologies, such as Robotic Process Automation (RPA) and Natural Language Processing (NLP), are pivotal in revolutionizing claims processing within the insurance sector. By leveraging these tools, insurers can automate repetitive tasks like data extraction and validation, significantly reducing human error and boosting accuracy. This shift allows employees to concentrate on more intricate tasks that demand critical thinking and direct customer interaction.
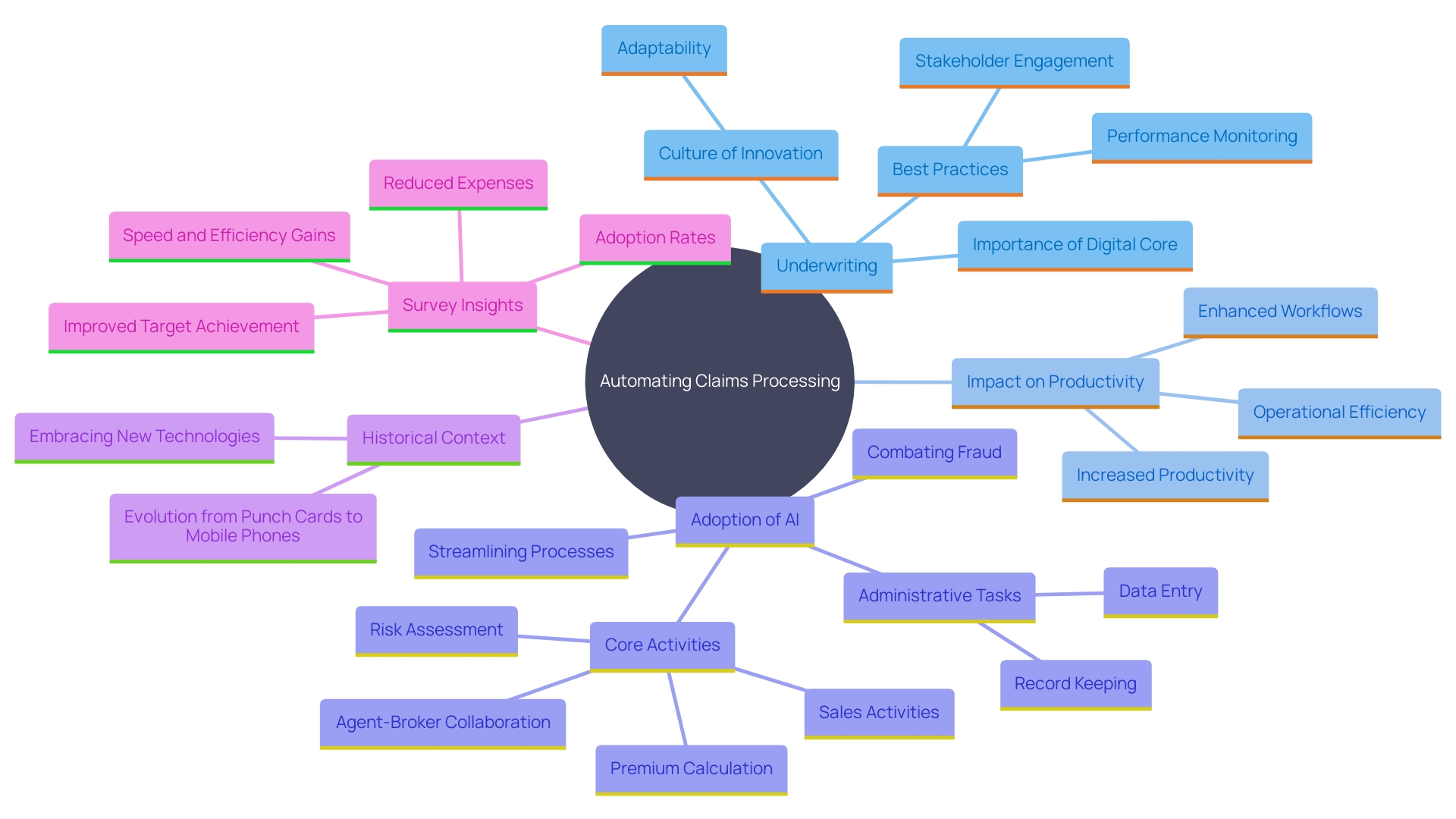
The influence of AI in the coverage sector is already evident. Research indicates that although 91% of insurance leaders have initiated AI proofs of concept, only 36% have fully integrated these technologies across their operations. Yet, those who have implemented AI, including RPA and NLP, report substantial improvements in speed, cost reduction, and goal achievement. For instance, underwriters traditionally spend over 40% of their time on administrative tasks, but with automation, this time is significantly cut down, allowing them to focus more on core activities like risk assessment and premium calculation.
Moreover, automated data entry powered by machine learning and NLP can lead to a 95% reduction in data entry time. This efficiency not only improves operational performance but also enables adjusters to provide superior service to clients. As the generative AI revolution progresses, the sector stands to benefit greatly from embracing these advanced technologies.
Case Study: A Nordic Insurance Company’s Automation Journey
A prominent Nordic insurance firm embarked on a journey to modernize its processing system to enhance efficiency and customer satisfaction. By conducting a comprehensive analysis of their current processes, they pinpointed critical areas ripe for automation. ‘Implementing Robotic Process Automation (RPA) and integrating machine learning algorithms led to a significant achievement: a reduction of over 40% in the average time taken to process requests.’. This transformation was made possible through a collaborative effort between the IT and claims departments, ensuring a smooth transition and continuous improvement.
‘The strides made by this coverage provider echo the broader industry trends.’. For instance, Cognizant’s collaboration with Alm. Brand Group in Denmark intends to automate various traditionally manual and repetitive tasks, including policy management and administrative duties, to increase efficiency and improve customer experience. Such initiatives underscore the potential of automation to revolutionize the sector by streamlining workflows and driving productivity gains.
Automation in underwriting also showcases similar benefits. By leveraging AI and rule-based systems, insurers can quickly analyze and process data, eliminating the need for tedious manual work and significantly enhancing operational efficiency. A broad survey highlights that 77% of senior executives are in some stage of adopting AI, reflecting a widespread recognition of its transformative potential.
These advancements are part of a larger shift within the sector towards embracing modern technologies to remain competitive and meet changing client expectations. With automation, firms in the sector not only enhance their operational efficiency but also establish a new benchmark for customer service in the digital era.
Benefits of Automated Claims Processing: Efficiency and Customer Satisfaction
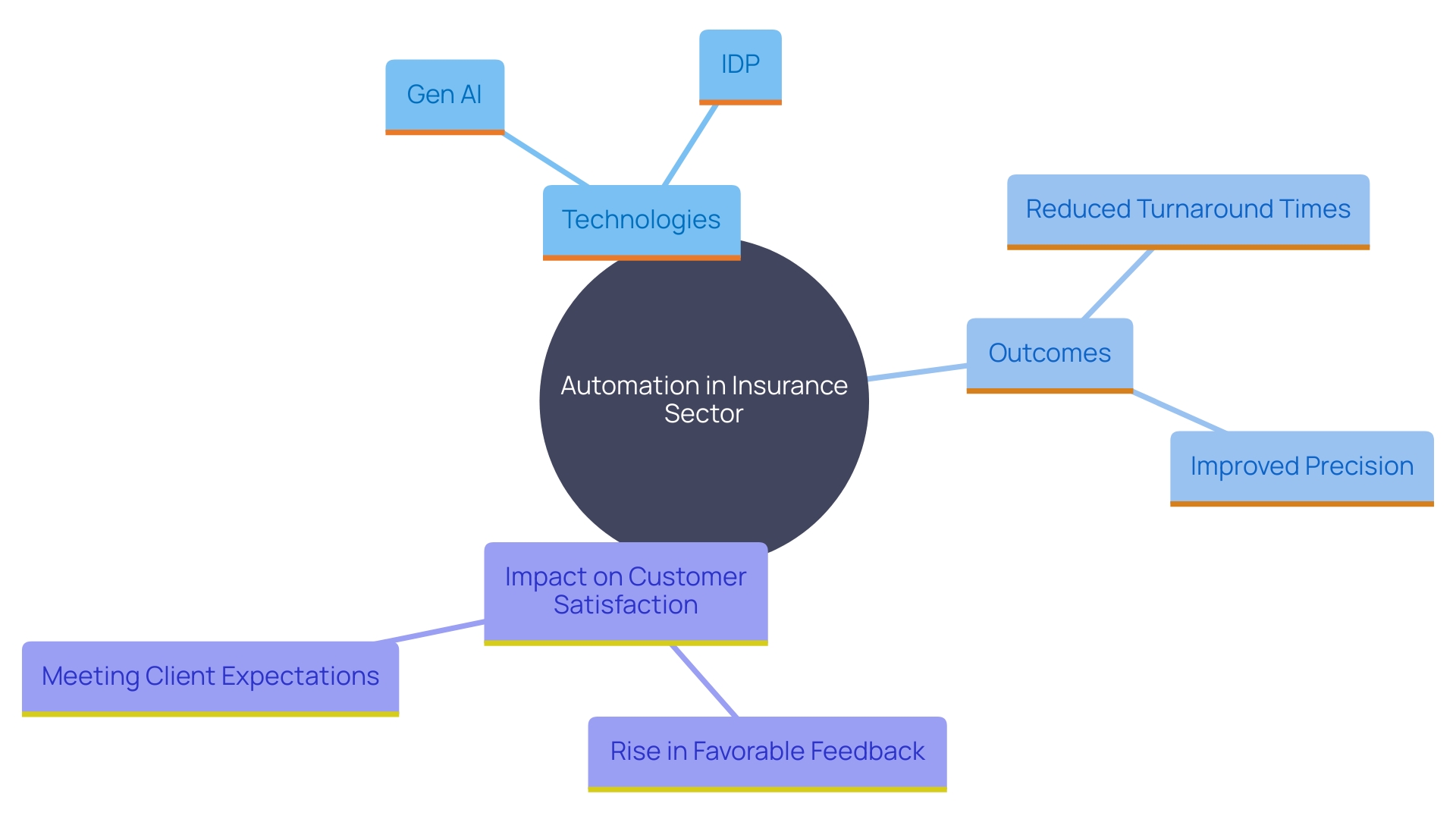
The implementation of automation in processing has transformed the Nordic insurance company, achieving remarkable results. Utilizing generative artificial intelligence (Gen AI) and intelligent document processing (IDP), the company significantly reduced turnaround times and improved precision in managing requests. According to a survey by Sollers Consulting and Ipsos, quicker claims processing is a critical priority for clients, with 52% to 63% citing prompt responses as a top expectation. Automation assisted the company in fulfilling these demands, resulting in a 30% rise in favorable feedback and enhanced satisfaction scores. ‘The implementation of AI not only streamlined operations but also provided valuable insights by analyzing patterns, thus improving the overall customer experience.’.
Key Technologies for Claims Automation: OCR, NLP, and RPA
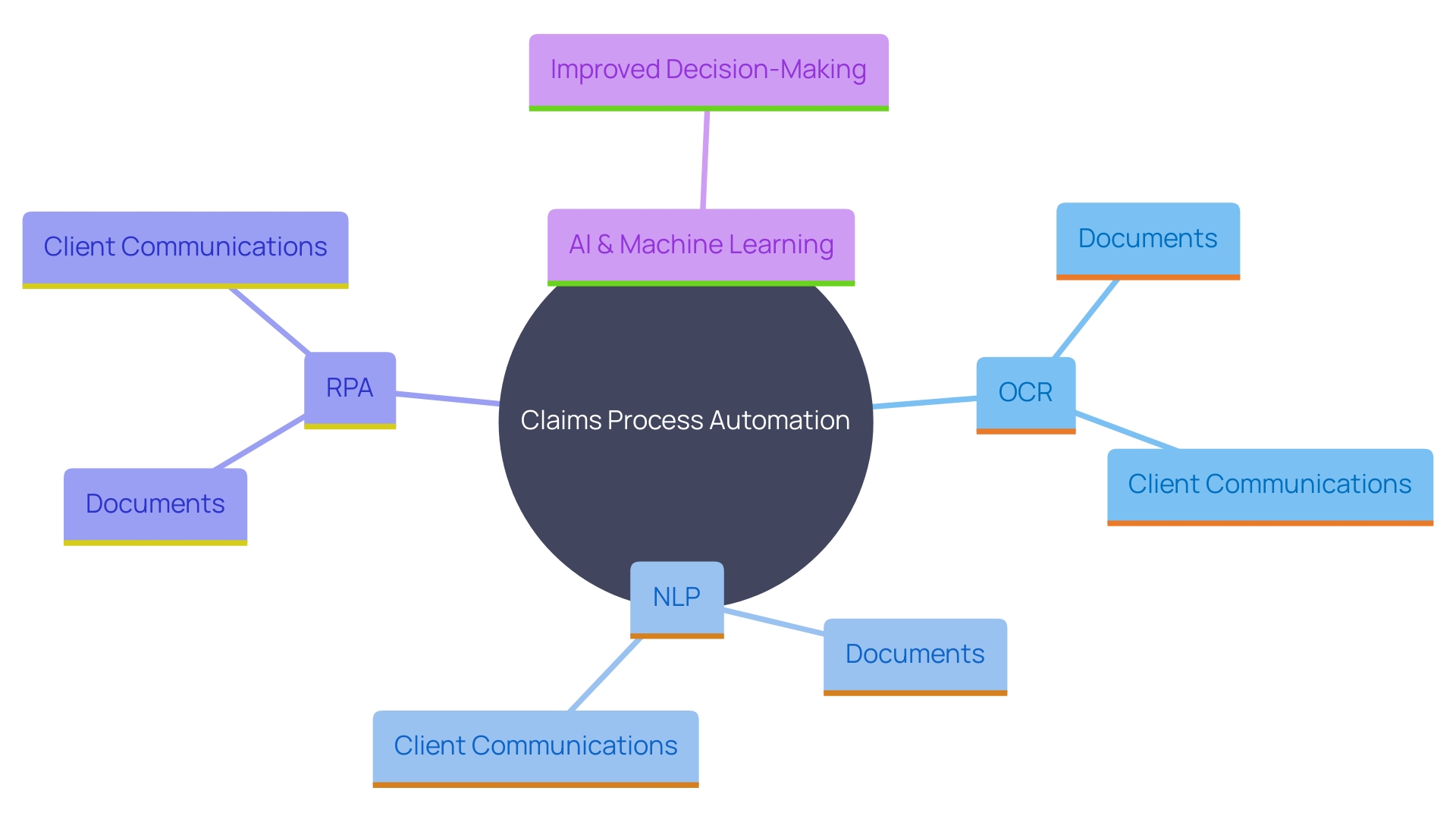
Successful claims process automation leverages several key technologies to optimize efficiency and accuracy. Optical Character Recognition (OCR) is essential in extracting information from various document types, including handwritten notes, tax returns, and medical records, transforming them into digitally editable formats. This technology is commonly utilized in healthcare and coverage areas for automated information entry and document digitization, minimizing manual mistakes and time usage.
‘Natural Language Processing (NLP) plays a crucial role in comprehending unstructured information, such as client communications and insurance claims, facilitating more accurate and efficient processing.’. By transforming complex text into organized information, NLP improves the capacity to analyze and respond to customer inquiries promptly.
Robotic Process Automation (RPA) automates repetitive, rule-based tasks, such as input and validation, by seamlessly integrating information across different systems. This integration is particularly beneficial in the underwriting process, where it accelerates workflows, minimizes errors, and boosts productivity.
Integrating these technologies creates a strong structure for effective management of requests, allowing organizations to handle substantial amounts of information precisely and quickly. As highlighted by industry experts, the adoption of AI and machine learning further enhances these capabilities, addressing the challenges associated with mixed structured and unstructured data, ultimately driving better decisions and outcomes.
Results and Impact: Reduced TAT, Improved Accuracy, and Enhanced Customer Experience
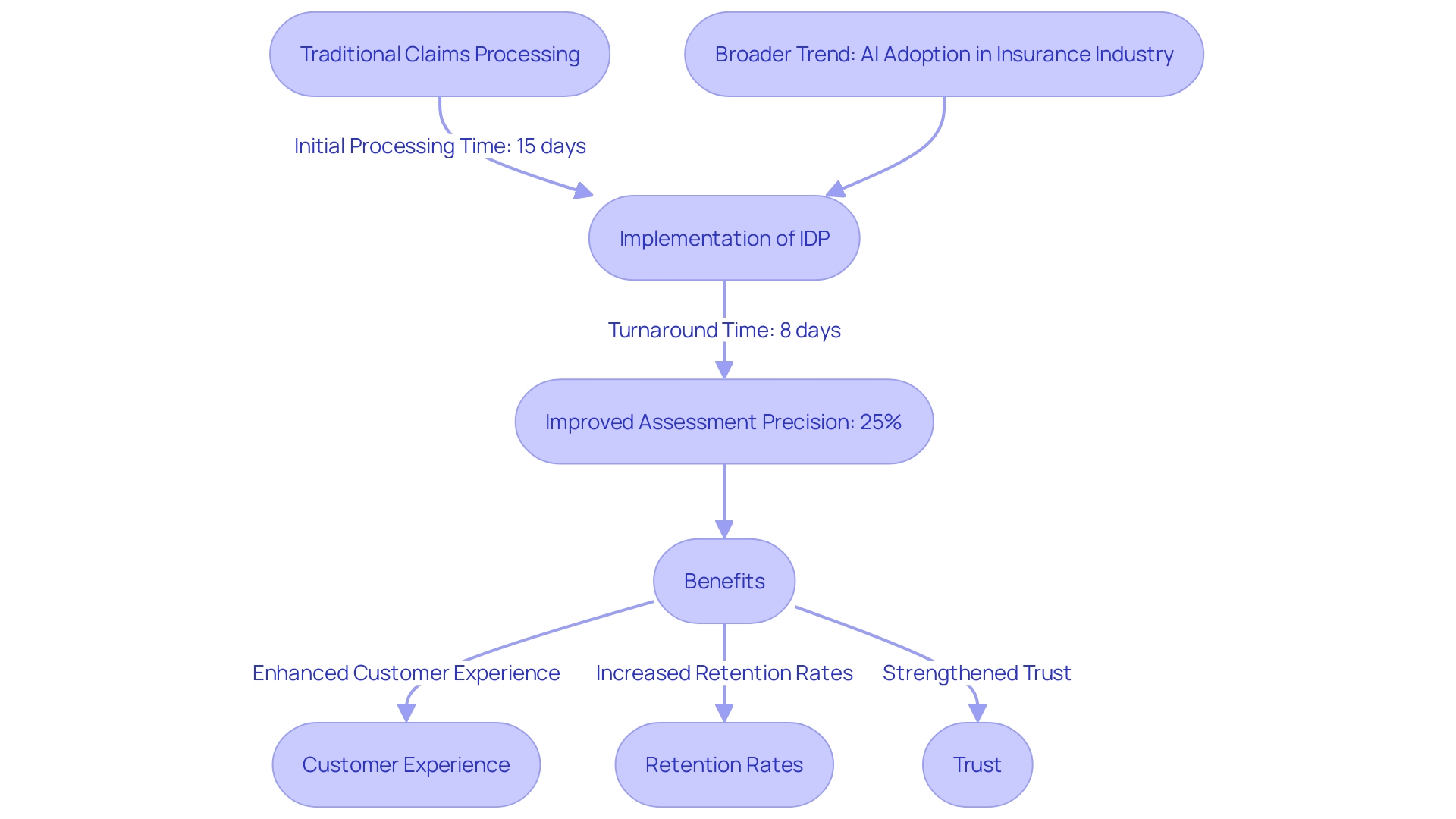
The Nordic insurance firm’s implementation of intelligent document processing (IDP) has transformed its processing operations. By utilizing this technology, the company reduced the average turnaround time (TAT) from 15 days to just 8 days while achieving a 25% improvement in the precision of assessment results. This transformation highlights the potential of IDP, which assists in extracting vital information from unstructured data, allowing insurers to handle requests more efficiently and effectively.
The enhanced accuracy and speed in processing claims have significantly improved the customer experience, resulting in higher retention rates and increased trust in the company’s services. This aligns with the broader trend in the insurance industry, where companies are increasingly adopting AI and automation to gain a competitive edge. According to Forrester, the right solutions can provide a substantial advantage, particularly in data analysis, which is crucial for success.
Moreover, the benefits of automation extend beyond operational performance to customer satisfaction. As the technology continues to evolve, its impact on the sector is expected to grow, promising even greater efficiency, accuracy, and overall operational effectiveness. This case demonstrates that with a clear vision and the right tools, companies can lead the way in digital transformation, reaping significant rewards in the process.
Lessons Learned and Best Practices for Claims Process Automation
Automating claims processing provides significant insights for organizations embarking on similar ventures. A notable example from the risk management sector is the transformation observed in underwriting processes. Traditionally manual and error-prone, underwriting has been revolutionized by automation, enhancing productivity and operational efficiency. This shift underscores the importance of establishing a strong digital core, as evidenced by the success of platforms like Salesforce and Microsoft in facilitating customer service and internal collaboration.
Key best practices for automation initiatives include engaging stakeholders early, maintaining clear communication, and continuously monitoring performance metrics. For example, in the area of AI adoption, 91% of financial services and protection leaders have launched AI proofs of concept, though only 36% have implemented them widely across business functions. This highlights the need for a balanced approach, combining technological innovation with well-defined rules and regulations to ensure sustainable digital transformations.
Fostering a culture of innovation and adaptability is crucial to fully leverage the benefits of automation. Investing in employee training is also essential, equipping staff to manage new technologies effectively. This approach not only improves job satisfaction but also addresses the challenges of processing large volumes of complex data, as seen in the case of AI and machine learning applications in the insurance industry. Through these strategies, organizations can drive better decisions and outcomes, ultimately achieving greater efficiency and productivity.
Conclusion
The transformation of claims processing through automation and AI technologies marks a significant shift in the insurance industry. Traditional methods, characterized by manual data entry and long response times, have proven inadequate in meeting modern customer expectations. By embracing automation, insurers can streamline workflows, enhance accuracy, and significantly reduce operational costs.
The collaboration between companies like Cognizant and Alm. Brand Group exemplifies how leveraging automation can lead to remarkable improvements in efficiency and customer satisfaction.
Key technologies such as Optical Character Recognition (OCR), Natural Language Processing (NLP), and Robotic Process Automation (RPA) serve as vital components in this transformation. These tools not only minimize human error but also free up employees to focus on more complex tasks that require critical thinking and direct customer engagement. As demonstrated by the Nordic insurance company’s successful implementation of intelligent document processing, organizations can achieve substantial reductions in turnaround times and improvements in claim accuracy, ultimately leading to higher customer retention and satisfaction.
The lessons learned from these automation initiatives underscore the importance of strategic planning, stakeholder engagement, and continuous performance monitoring. Fostering a culture of innovation and investing in employee training are crucial for maximizing the benefits of automation. As the insurance sector continues to evolve, those who adopt these advanced technologies will be well-positioned to meet the challenges of an increasingly competitive market while delivering exceptional service to their customers.

