Introduction
In the ever-evolving healthcare landscape, the prior authorization process stands as a critical yet challenging hurdle for providers and patients alike. This essential mechanism ensures that necessary treatments are approved by insurance companies, safeguarding patient care while managing costs.
However, the complexities and delays associated with prior authorization can hinder timely access to medical services, leaving healthcare professionals grappling with administrative burdens. As the demand for efficiency grows, innovative solutions such as Robotic Process Automation (RPA) and Artificial Intelligence (AI) are emerging as powerful tools to streamline these workflows.
By embracing automation, healthcare organizations can not only reduce wait times and errors but also enhance compliance and improve patient experiences. This article delves into the importance of prior authorization, the challenges it presents, and the transformative potential of automation in reshaping the future of healthcare delivery.
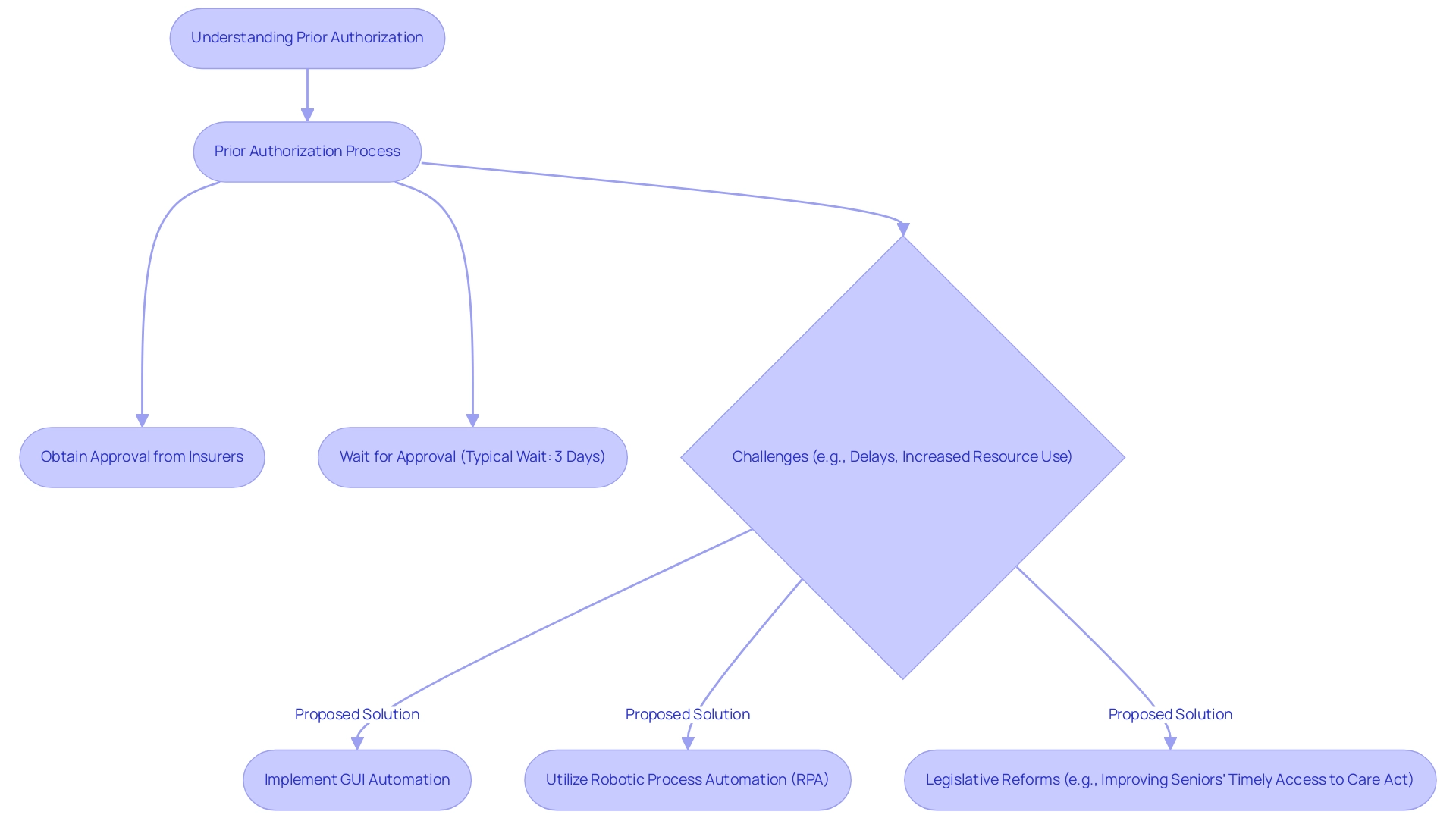
Understanding Prior Authorization: Importance and Challenges
Advance approval plays a crucial role in the medical field, requiring providers to obtain consent from insurance firms before offering certain services or medications. This process is crucial for ensuring that patients receive necessary care while allowing insurers to manage costs effectively. However, the complexities of this system can significantly hinder patient care.
Studies show that the typical wait duration for previous approvals is three days, with 31% of medical professionals facing delays longer than a week. The American Medical Association (AMA) emphasizes that 86% of doctors think that previous approval frequently results in increased use of healthcare resources, contributing to the administrative load on providers. To combat these challenges, implementing GUI automation and Robotic Process Automation (RPA) can help automate prior authorization, reducing wait times and enhancing operational efficiency.
For example, a mid-sized company that implemented GUI automation decreased data entry errors by 70% and sped up testing activities by 50%, achieving ROI within six months. Legislative efforts, such as the ASTRO-supported Improving Seniors’ Timely Access to Care Act of 2024, aim to reform these processes by establishing a real-time decision-making framework for Medicare Advantage plans. As medical leaders advocate for timely responses, the AMA proposes a 48-hour determination for nonurgent care and 24 hours for urgent care.
These specific timeframes underscore the necessity of integrating tailored AI solutions and business intelligence systems to automate prior authorization, alleviate delays, and ultimately enhance the operational efficiency of healthcare delivery.
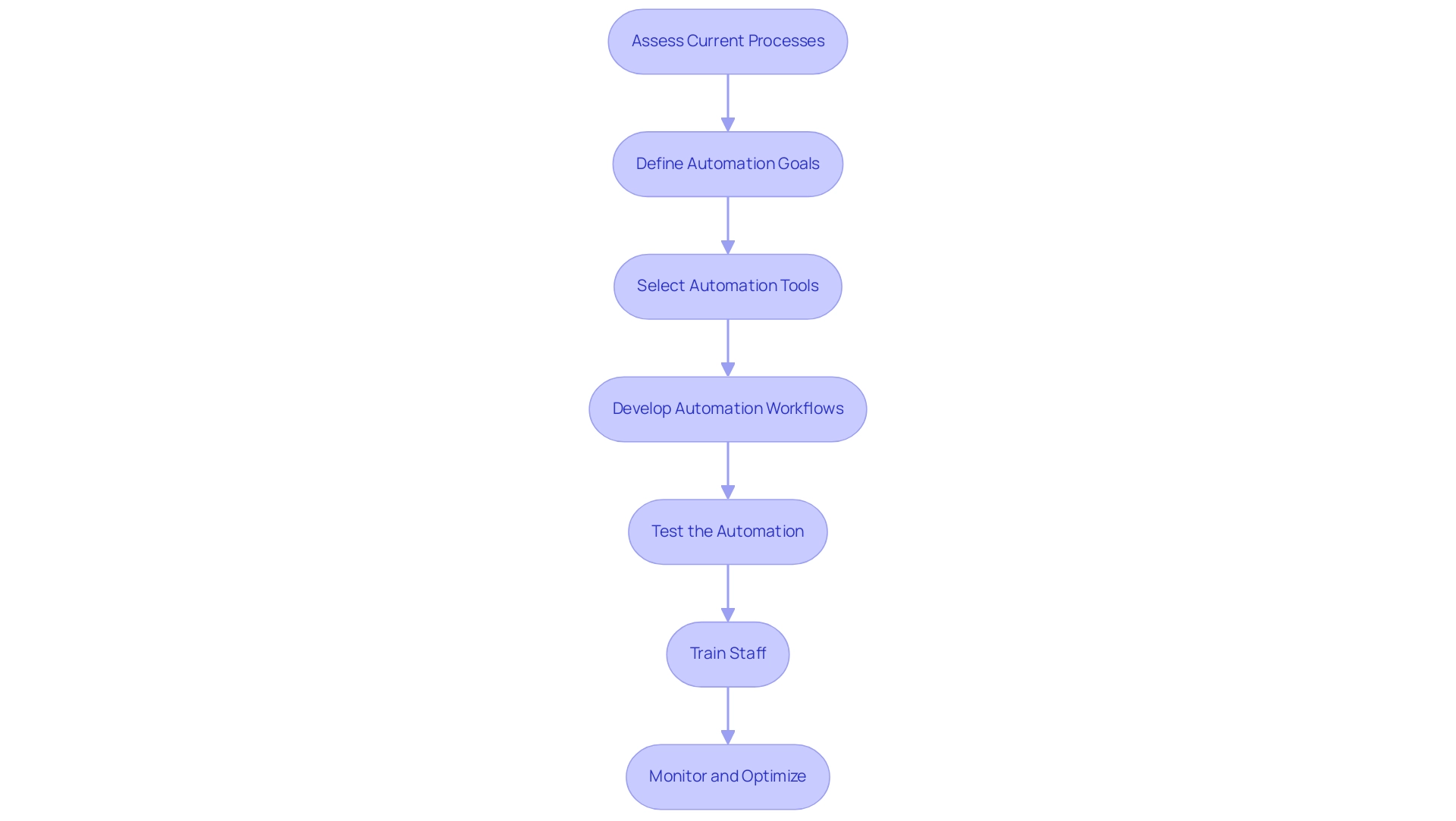
Step-by-Step Guide to Automating Prior Authorization
-
Assess Current Processes: Begin by carefully outlining your existing pre-approval workflows. Identify bottlenecks and common errors, particularly those that require frequent manual intervention. Recognizing these pain points is crucial to understanding where we can automate prior authorization to alleviate the exhaustion caused by repetitive tasks.
-
Define Automation Goals: Set clear, measurable objectives for your automation initiative. Whether your aim is to reduce approval times or minimize the paperwork burden, having defined goals will guide your strategy to automate prior authorization, helping measure success while also addressing the emotional fatigue of your team.
-
Select Automation Tools: Conduct thorough research to identify the right Robotic Process Automation (RPA) tools, such as EMMA RPA and Microsoft Power Automate, that align with your goals. These innovative solutions are designed to enhance efficiency and employee morale by automating repetitive tasks, including the ability to automate prior authorization, and streamlining workflows. Prioritize tools that offer seamless integration with your existing systems, ensuring a smoother transition to automated workflows, which can help modernize outdated systems that hinder operations.
-
Develop Automation Workflows: Design specific automation workflows that detail how tasks will be executed. This includes automating data entry, document submission, and follow-up communications. A well-defined workflow is essential for effective processes that can automate prior authorization and improve efficiency, helping to alleviate the burden of manual tasks on your staff.
-
Test the Automation: Prior to full implementation, engage in pilot testing to validate that your automation solutions function as intended. Use feedback from these tests to make necessary adjustments before scaling up, ensuring that the solutions effectively address the challenges posed by staffing shortages.
-
Train Staff: Equip your team with the necessary training to effectively operate the new automated systems. Ensuring that staff are comfortable with the changes is critical for the success of your automation efforts and can significantly improve employee satisfaction by reducing their workload.
-
Monitor and Optimize: After implementation, it’s essential to continuously oversee the performance of your automated systems. Utilize data-driven insights to automate prior authorization and make ongoing adjustments that enhance efficiency and effectiveness. Recent statistics suggest that 86% of doctors believe that previous approvals result in higher healthcare resource use; therefore, improving your methods can greatly alleviate this challenge, boosting overall workflow efficiency. Moreover, recent administrative measures regarding previous approvals seek to elucidate standards for Medicare Advantage plans and enhance electronic systems, which coincides with your automation objectives. As mentioned by CMS, these changes are aimed at streamlining procedures and reducing provider burdens. Furthermore, grasping the variability in previous approval requests, with Humana having the highest at 2.9 requests per enrollee and Kaiser Permanente the lowest at 0.5, emphasizes the need for customized automation strategies across various medical environments.
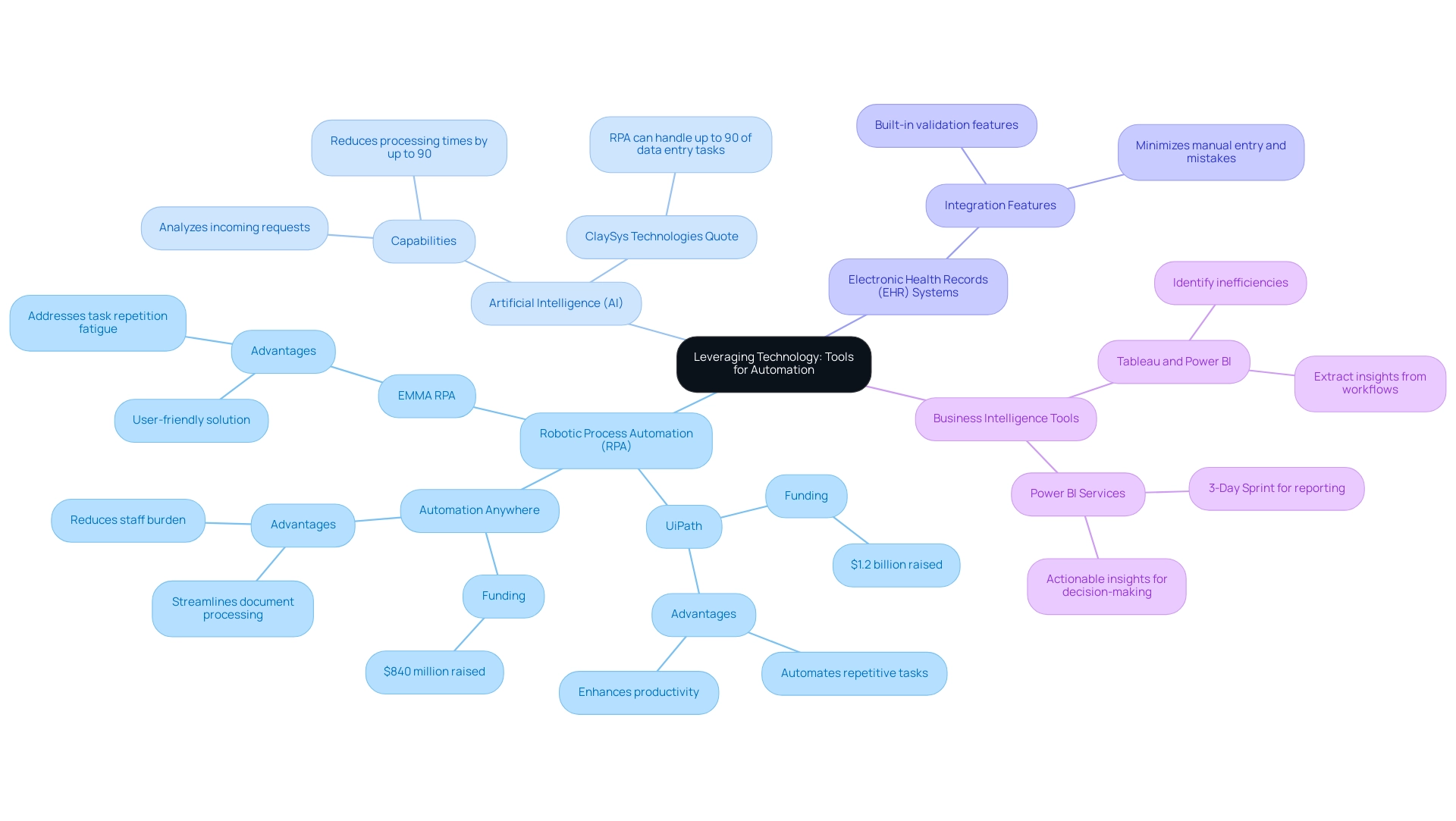
Leveraging Technology: Tools for Automation
A variety of innovative tools is available to streamline and automate the previous approval procedure, significantly enhancing operational efficiency:
-
Robotic Process Automation (RPA): Leading platforms such as UiPath and Automation Anywhere excel at automating repetitive tasks, including data entry and document processing, alleviating the burden on staff. Notably, UiPath raised $1.2 billion and Automation Anywhere secured $840 million in funding, underscoring the growing importance of RPA technologies in the healthcare sector. Our own EMMA RPA provides a user-friendly solution that enhances productivity and employee morale by taking over mundane tasks, allowing your team to focus on higher-value work. EMMA RPA specifically addresses task repetition fatigue and staffing shortages, making it an essential tool for modern operations.
-
Artificial Intelligence (AI): AI-driven solutions revolutionize the handling of incoming requests by analyzing them against predefined eligibility criteria. This capability can reduce processing times by up to 90%, as noted by experts from ClaySys Technologies, who state that RPA can handle up to 90% of data entry tasks in clinical research. Our customized AI solutions, featuring Small Language Models and interactive GenAI Workshops, provide your team with the abilities to utilize AI efficiently in their workflows, enhancing data quality and operational effectiveness.
-
Electronic Health Records (EHR) Systems: Numerous contemporary EHR systems now integrate built-in previous validation features, allowing smooth submission methods directly from patient records, thus minimizing manual entry and mistakes. This integration not only simplifies operations but also improves data precision.
-
Business Intelligence Tools: Using solutions like Tableau or Power BI assists organizations in extracting insights from their previous approval workflows, identifying inefficiencies and uncovering opportunities for enhancement. Our Power BI services guarantee efficient reporting and actionable insights, with a 3-Day Sprint aimed at swiftly producing professionally crafted reports that can inform decision-making.
By adopting these technologies, organizations in the medical field can automate prior authorization, enhance their operational workflows, ensure timely approvals, and improve overall patient care and satisfaction. Additionally, with automation expected to save £17 billion off public sector payments by 2030 compared to 2015, the financial benefits of these innovations are substantial.
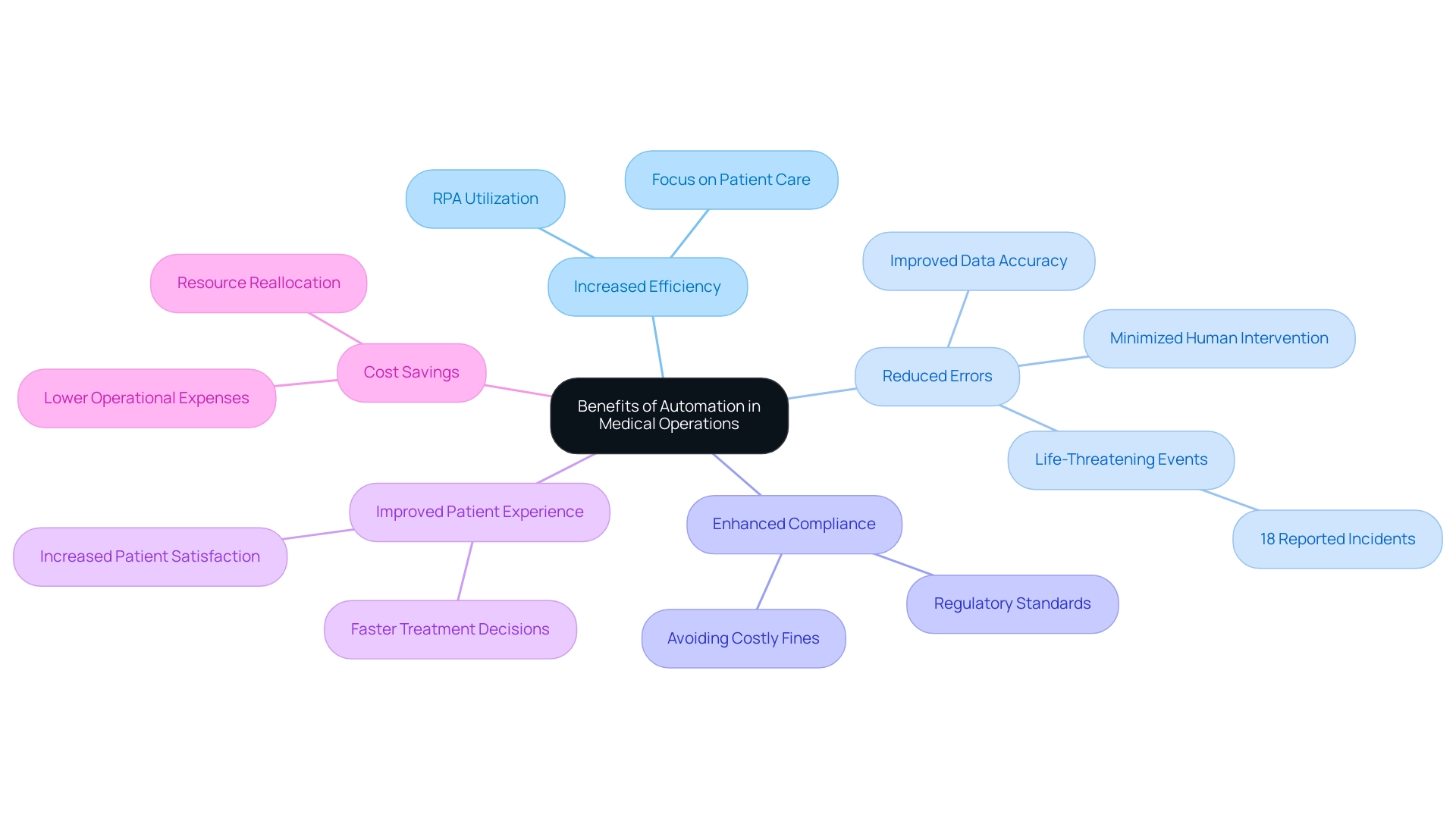
Benefits of Automation: Enhancing Efficiency and Reducing Burdens
Automating the prior authorization procedure offers numerous benefits that can revolutionize medical operations:
- Increased Efficiency: By utilizing Robotic Process Automation (RPA), medical providers can significantly decrease the time dedicated to manual tasks, enabling teams to concentrate on patient care instead of documentation. This shift is essential in today’s fast-paced medical environment, where operational efficiency is paramount.
- Reduced Errors: Automation minimizes human intervention, significantly lowering the risk of errors in data entry and documentation. This leads to more accurate and reliable submissions, ultimately enhancing the quality of care. Alarmingly, 18% of medical professionals report that manual methods have resulted in life-threatening situations or necessitated urgent interventions to prevent lasting damage.
- Enhanced Compliance: Automated systems can be meticulously programmed to meet regulatory standards, ensuring that all necessary documentation complies with current requirements. This proactive approach helps organizations avoid costly fines and maintain their reputations.
- Improved Patient Experience: Streamlined prior authorization processes facilitate faster treatment decisions, greatly enhancing the overall patient experience and satisfaction. When patients obtain prompt approvals, they are more inclined to interact positively with their providers.
- Cost Savings: The decrease of administrative burdens not only lowers operational expenses but also enables organizations to allocate resources more effectively. This strategic reallocation can lead to improved patient outcomes and organizational sustainability.
Moreover, integrating tailored AI solutions alongside RPA can further enhance automation efforts by providing insights that cut through the complexities of the evolving AI landscape. These solutions enable medical organizations to make data-driven decisions, ultimately driving growth and innovation. As emphasized by industry leaders, utilizing automation tools to automate prior authorization and simplify the previous approval workflow is an excellent starting point. With legislative efforts pushing for quicker payer turnaround times, such as those outlined in the case study on ‘Legislative Efforts and Automation Adoption,’ organizations aiming to thrive in the evolving landscape must automate prior authorization as a crucial step. Additionally, instructing participants about the previous approval system and its criteria can greatly enhance comprehension and adherence, further boosting the efficiency of automation in medical services.
The Future of Prior Authorization: Trends and Predictions
The landscape of prior authorization automation is on the brink of remarkable transformation, driven by several pivotal trends:
-
Increased Integration of AI and RPA: The continuous evolution of AI technologies, alongside Robotic Process Automation (RPA), is set to create a more seamless integration into prior authorization processes. This advancement will not only accelerate decision-making but will also enhance accuracy, ensuring that approvals are timely and precise. The AI in drug discovery market is anticipated to achieve USD 12.8 billion by 2032, with a CAGR of 27.5% from 2023 to 2032, signaling a robust trend towards AI and RPA integration in the medical sector.
-
Data-Driven Decision Making: Organizations are increasingly leveraging analytics and business intelligence to guide their prior authorization strategies. This reliance on data empowers service providers to proactively manage workflows, leading to more efficient operations and better resource allocation, ultimately driving growth and innovation.
-
Enhanced Interoperability: The push for improved interoperability among medical systems is crucial. By enabling smoother data exchanges through RPA, organizations can considerably lessen delays in previous approvals, improving patient care and operational efficiency.
-
Focus on Patient-Centric Solutions: The medical field is progressively shifting towards solutions that prioritize the patient experience. Innovations focused on simplifying previous approval processes are emerging, intended to enhance outcomes and promote a more caring medical delivery model. Notably, 68% of non-users of AI technologies are Gen X or Baby Boomers, highlighting the generational gap in AI adoption that organizations must consider in their patient-centric approaches. Additionally, the case study titled “AI Demographics by Age” illustrates that while 30.8% of individuals aged 61+ use virtual assistants weekly, younger age groups show lower engagement, emphasizing the need for tailored solutions across diverse patient demographics.
Manual, repetitive tasks can significantly slow down operations, leading to wasted time and resources. By leveraging RPA, organizations can automate prior authorization tasks, streamline workflows, and enhance overall efficiency. Specific applications of RPA in previous approvals include automated data entry, real-time status updates, and intelligent document processing, which collectively reduce processing times and enhance accuracy.
By leveraging these trends, particularly the integration of RPA and AI, organizations can effectively position themselves to adapt and flourish in an evolving healthcare environment, harnessing the power of technology to automate prior authorization frameworks.

Conclusion
The prior authorization process remains a crucial component of healthcare, ensuring that patients receive necessary treatments while helping insurers manage costs. However, the challenges it presents—such as lengthy wait times and administrative burdens—demand innovative solutions. Embracing automation through Robotic Process Automation (RPA) and Artificial Intelligence (AI) can significantly streamline these processes, enhancing efficiency and reducing errors.
Implementing automation not only alleviates the workload on healthcare providers but also improves patient experiences by expediting treatment decisions. By carefully assessing current workflows, defining clear automation goals, and selecting the right tools, healthcare organizations can create a more efficient prior authorization process. The integration of AI and RPA is essential for driving data-driven decision-making and enhancing operational workflows, ultimately leading to better resource allocation and patient outcomes.
As the healthcare landscape evolves, the push for automation in prior authorization is not just a trend but a necessary step toward a more efficient and patient-centric system. By leveraging technology to reduce delays and improve compliance, healthcare organizations can position themselves for success in a rapidly changing environment. Embracing these solutions will not only enhance operational efficiency but also foster a healthcare delivery model that prioritizes timely care and patient satisfaction. The future of healthcare relies on the ability to adapt and innovate, making automation a vital investment for organizations aiming to thrive in this landscape.

